By the end of this section, you will be able to:
An important way to understand the effects of native neurochemicals in the autonomic system is in considering the effects of pharmaceutical drugs. This can be considered in terms of how drugs change autonomic function. These effects will primarily be based on how drugs act at the receptors of the autonomic system neurochemistry. The signaling molecules of the nervous system interact with proteins in the cell membranes of various target cells. In fact, no effect can be attributed to just the signaling molecules themselves without considering the receptors. A chemical that the body produces to interact with those receptors is called an endogenous chemical, whereas a chemical introduced to the system from outside is an exogenous chemical. Exogenous chemicals may be of a natural origin, such as a plant extract, or they may be synthetically produced in a pharmaceutical laboratory.
One important drug that affects the autonomic system broadly is not a pharmaceutical therapeutic agent associated with the system. This drug is nicotine. The effects of nicotine on the autonomic nervous system are important in considering the role smoking can play in health.
All ganglionic neurons of the autonomic system, in both sympathetic and parasympathetic ganglia, are activated by ACh released from preganglionic fibers. The ACh receptors on these neurons are of the nicotinic type, meaning that they are ligand-gated ion channels. When the neurotransmitter released from the preganglionic fiber binds to the receptor protein, a channel opens to allow positive ions to cross the cell membrane. The result is depolarization of the ganglia. Nicotine acts as an ACh analog at these synapses, so when someone takes in the drug, it binds to these ACh receptors and activates the ganglionic neurons, causing them to depolarize.
Ganglia of both divisions are activated equally by the drug. For many target organs in the body, this results in no net change. The competing inputs to the system cancel each other out and nothing significant happens. For example, the sympathetic system will cause sphincters in the digestive tract to contract, limiting digestive propulsion, but the parasympathetic system will cause the contraction of other muscles in the digestive tract, which will try to push the contents of the digestive system along. The end result is that the food does not really move along and the digestive system has not appreciably changed.
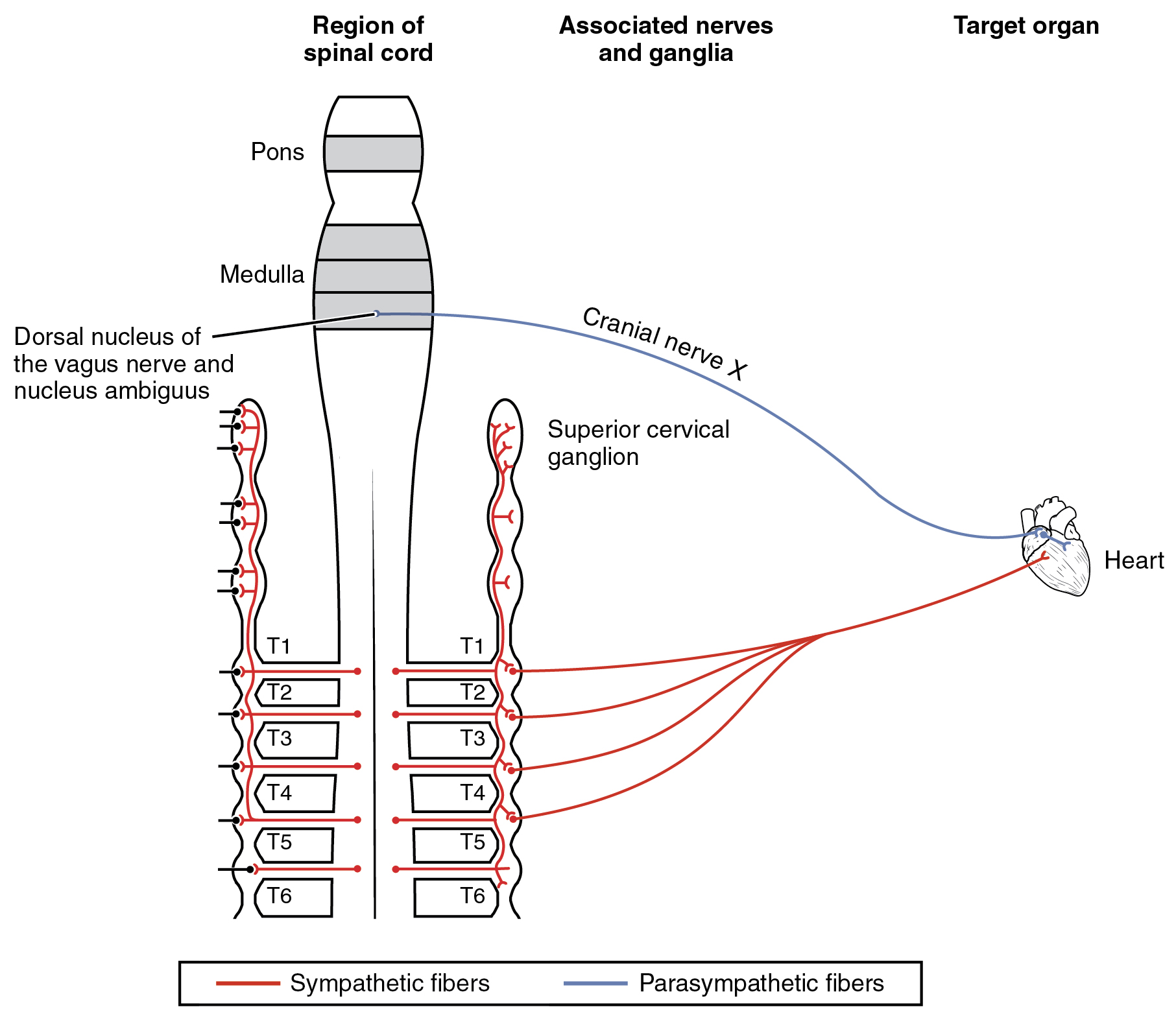
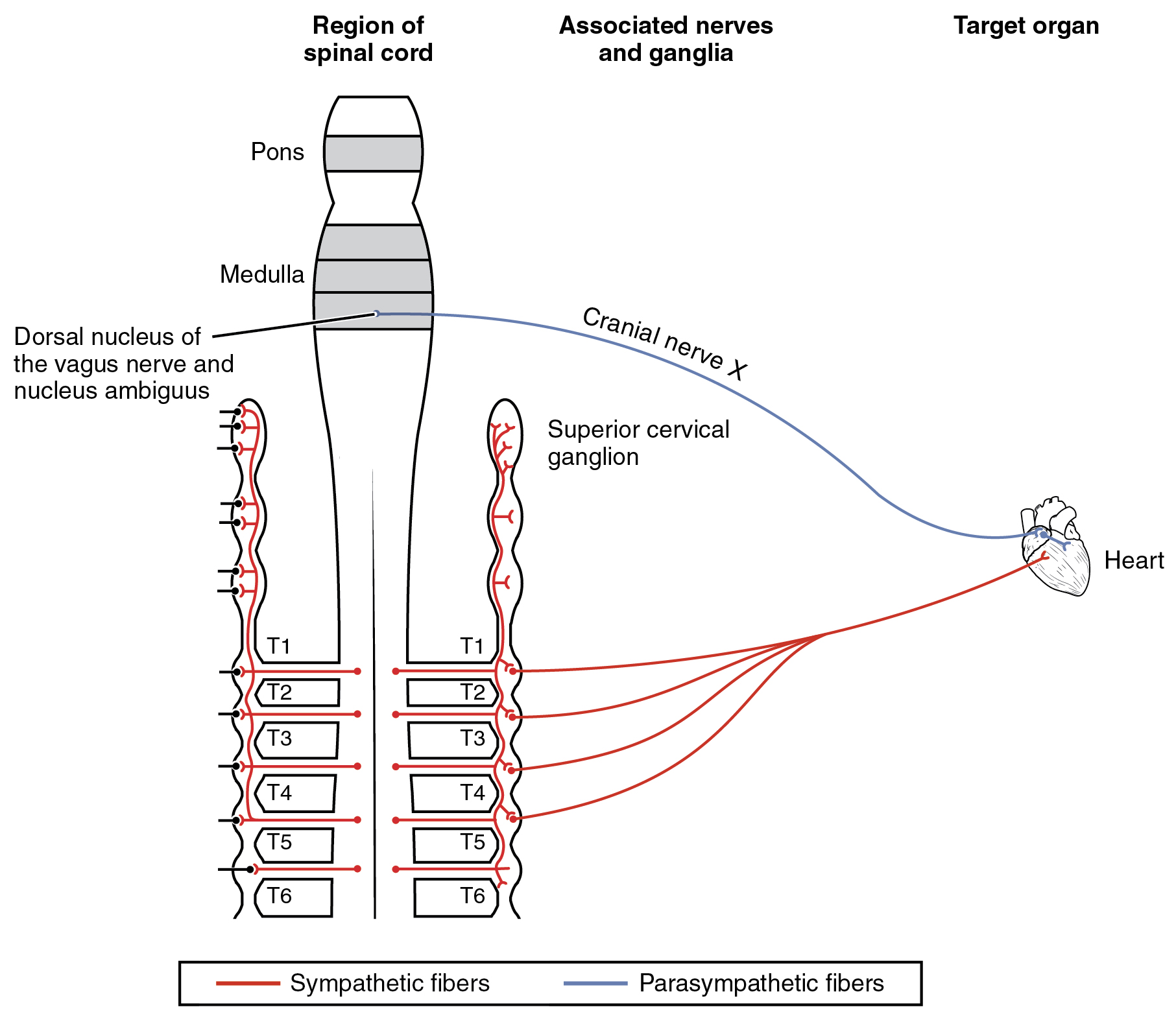
The system in which this can be problematic is in the cardiovascular system, which is why smoking is a risk factor for cardiovascular disease. First, there is no significant parasympathetic regulation of blood pressure. Only a limited number of blood vessels are affected by parasympathetic input, so nicotine will preferentially cause the vascular tone to become more sympathetic, which means blood pressure will be increased. Second, the autonomic control of the heart is special. Unlike skeletal or smooth muscles, cardiac muscle is intrinsically active, meaning that it generates its own action potentials. The autonomic system does not cause the heart to beat, it just speeds it up (sympathetic) or slows it down (parasympathetic). The mechanisms for this are not mutually exclusive, so the heart receives conflicting signals, and the rhythm of the heart can be affected ([link]).
The neurochemistry of the sympathetic system is based on the adrenergic system. Norepinephrine and epinephrine influence target effectors by binding to the α-adrenergic or β-adrenergic receptors. Drugs that affect the sympathetic system affect these chemical systems. The drugs can be classified by whether they enhance the functions of the sympathetic system or interrupt those functions. A drug that enhances adrenergic function is known as a sympathomimetic drug, whereas a drug that interrupts adrenergic function is a sympatholytic drug.
When the sympathetic system is not functioning correctly or the body is in a state of homeostatic imbalance, these drugs act at postganglionic terminals and synapses in the sympathetic efferent pathway. These drugs either bind to particular adrenergic receptors and mimic norepinephrine at the synapses between sympathetic postganglionic fibers and their targets, or they increase the production and release of norepinephrine from postganglionic fibers. Also, to increase the effectiveness of adrenergic chemicals released from the fibers, some of these drugs may block the removal or reuptake of the neurotransmitter from the synapse.
A common sympathomimetic drug is phenylephrine, which is a common component of decongestants. It can also be used to dilate the pupil and to raise blood pressure. Phenylephrine is known as an α1-adrenergic agonist, meaning that it binds to a specific adrenergic receptor, stimulating a response. In this role, phenylephrine will bind to the adrenergic receptors in bronchioles of the lungs and cause them to dilate. By opening these structures, accumulated mucus can be cleared out of the lower respiratory tract. Phenylephrine is often paired with other pharmaceuticals, such as analgesics, as in the “sinus” version of many over-the-counter drugs, such as Tylenol Sinus® or Excedrin Sinus®, or in expectorants for chest congestion such as in Robitussin CF®.
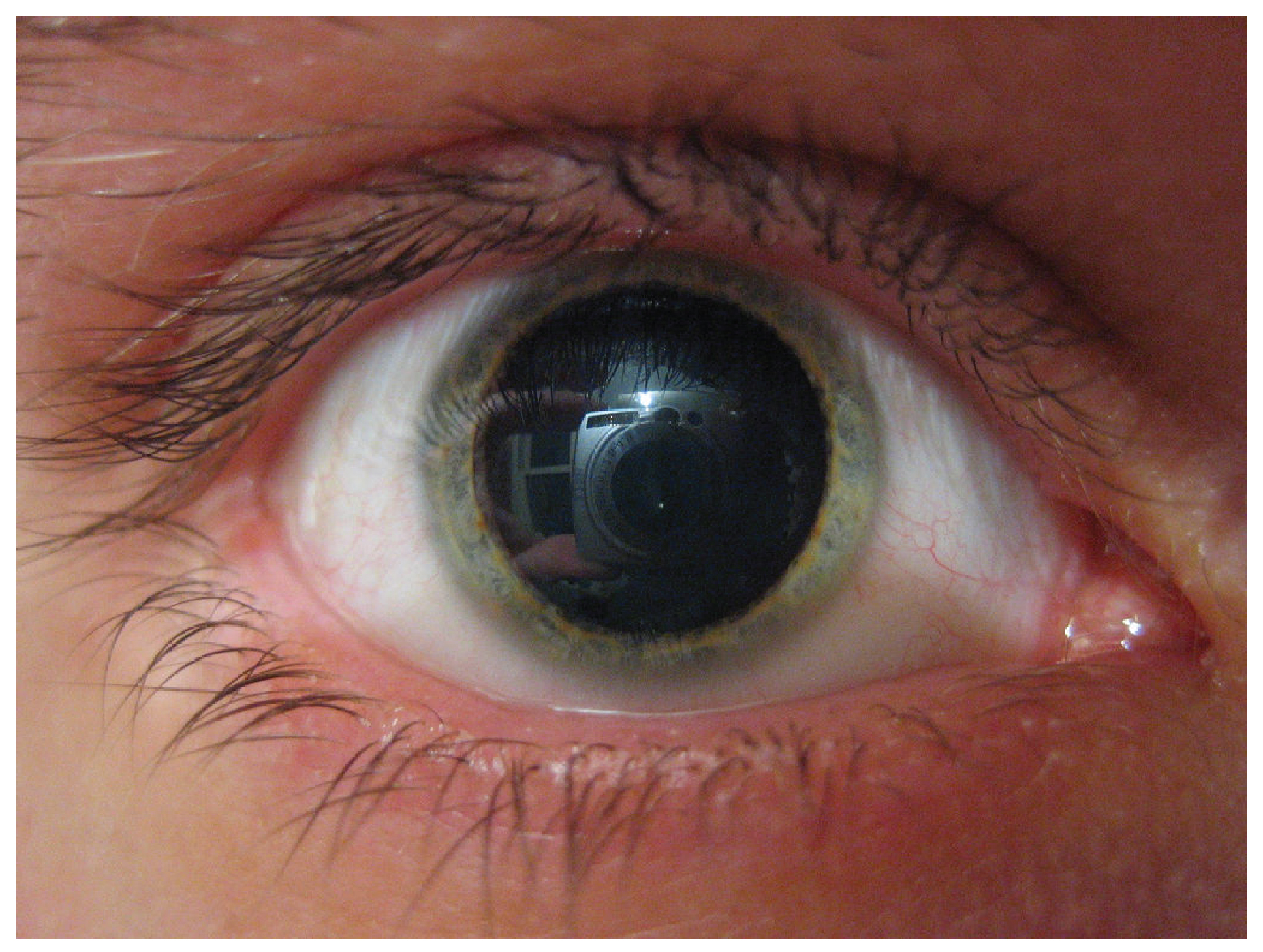
A related molecule, called pseudoephedrine, was much more commonly used in these applications than was phenylephrine, until the molecule became useful in the illicit production of amphetamines. Phenylephrine is not as effective as a drug because it can be partially broken down in the digestive tract before it is ever absorbed. Like the adrenergic agents, phenylephrine is effective in dilating the pupil, known as mydriasis ([link]). Phenylephrine is used during an eye exam in an ophthalmologist’s or optometrist’s office for this purpose. It can also be used to increase blood pressure in situations in which cardiac function is compromised, such as under anesthesia or during septic shock.
Other drugs that enhance adrenergic function are not associated with therapeutic uses, but affect the functions of the sympathetic system in a similar fashion. Cocaine primarily interferes with the uptake of dopamine at the synapse and can also increase adrenergic function. Caffeine is an antagonist to a different neurotransmitter receptor, called the adenosine receptor. Adenosine will suppress adrenergic activity, specifically the release of norepinephrine at synapses, so caffeine indirectly increases adrenergic activity. There is some evidence that caffeine can aid in the therapeutic use of drugs, perhaps by potentiating (increasing) sympathetic function, as is suggested by the inclusion of caffeine in over-the-counter analgesics such as Excedrin®.
Drugs that interfere with sympathetic function are referred to as sympatholytic, or sympathoplegic, drugs. They primarily work as an antagonist to the adrenergic receptors. They block the ability of norepinephrine or epinephrine to bind to the receptors so that the effect is “cut” or “takes a blow,” to refer to the endings “-lytic” and “-plegic,” respectively. The various drugs of this class will be specific to α-adrenergic or β-adrenergic receptors, or to their receptor subtypes.
Possibly the most familiar type of sympatholytic drug are the β-blockers. These drugs are often used to treat cardiovascular disease because they block the β-receptors associated with vasoconstriction and cardioacceleration. By allowing blood vessels to dilate, or keeping heart rate from increasing, these drugs can improve cardiac function in a compromised system, such as for a person with congestive heart failure or who has previously suffered a heart attack. A couple of common versions of β-blockers are metoprolol, which specifically blocks the β1-receptor, and propanolol, which nonspecifically blocks β-receptors. There are other drugs that are α-blockers and can affect the sympathetic system in a similar way.
Other uses for sympatholytic drugs are as antianxiety medications. A common example of this is clonidine, which is an α-agonist. The sympathetic system is tied to anxiety to the point that the sympathetic response can be referred to as “fight, flight, or fright.” Clonidine is used for other treatments aside from hypertension and anxiety, including pain conditions and attention deficit hyperactivity disorder.
Drugs affecting parasympathetic functions can be classified into those that increase or decrease activity at postganglionic terminals. Parasympathetic postganglionic fibers release ACh, and the receptors on the targets are muscarinic receptors. There are several types of muscarinic receptors, M1–M5, but the drugs are not usually specific to the specific types. Parasympathetic drugs can be either muscarinic agonists or antagonists, or have indirect effects on the cholinergic system. Drugs that enhance cholinergic effects are called parasympathomimetic drugs, whereas those that inhibit cholinergic effects are referred to as anticholinergic drugs.
Pilocarpine is a nonspecific muscarinic agonist commonly used to treat disorders of the eye. It reverses mydriasis, such as is caused by phenylephrine, and can be administered after an eye exam. Along with constricting the pupil through the smooth muscle of the iris, pilocarpine will also cause the ciliary muscle to contract. This will open perforations at the base of the cornea, allowing for the drainage of aqueous humor from the anterior compartment of the eye and, therefore, reducing intraocular pressure related to glaucoma.
Atropine and scopolamine are part of a class of muscarinic antagonists that come from the Atropa genus of plants that include belladonna or deadly nightshade ([link]). The name of one of these plants, belladonna, refers to the fact that extracts from this plant were used cosmetically for dilating the pupil. The active chemicals from this plant block the muscarinic receptors in the iris and allow the pupil to dilate, which is considered attractive because it makes the eyes appear larger. Humans are instinctively attracted to anything with larger eyes, which comes from the fact that the ratio of eye-to-head size is different in infants (or baby animals) and can elicit an emotional response. The cosmetic use of belladonna extract was essentially acting on this response. Atropine is no longer used in this cosmetic capacity for reasons related to the other name for the plant, which is deadly nightshade. Suppression of parasympathetic function, especially when it becomes systemic, can be fatal. Autonomic regulation is disrupted and anticholinergic symptoms develop. The berries of this plant are highly toxic, but can be mistaken for other berries. The antidote for atropine or scopolamine poisoning is pilocarpine.

| Sympathetic and Parasympathetic Effects of Different Drug Types | ||||
|---|---|---|---|---|
| Drug type | Example(s) | Sympathetic effect | Parasympathetic effect | Overall result |
| Nicotinic agonists | Nicotine | Mimic ACh at preganglionic synapses, causing activation of postganglionic fibers and the release of norepinephrine onto the target organ | Mimic ACh at preganglionic synapses, causing activation of postganglionic fibers and the release of ACh onto the target organ | Most conflicting signals cancel each other out, but cardiovascular system is susceptible to hypertension and arrhythmias |
| Sympathomimetic drugs | Phenylephrine | Bind to adrenergic receptors or mimics sympathetic action in some other way | No effect | Increase sympathetic tone |
| Sympatholytic drugs | β-blockers such as propanolol or metoprolol; α-agonists such as clonidine | Block binding to adrenergic drug or decrease adrenergic signals | No effect | Increase parasympathetic tone |
| Parasymphatho-mimetics/muscarinic agonists | Pilocarpine | No effect, except on sweat glands | Bind to muscarinic receptor, similar to ACh | Increase parasympathetic tone |
| Anticholinergics/muscarinic antagonists | Atropine, scopolamine, dimenhydrinate | No effect | Block muscarinic receptors and parasympathetic function | Increase sympathetic tone |
Autonomic Nervous System Approximately 33 percent of people experience a mild problem with motion sickness, whereas up to 66 percent experience motion sickness under extreme conditions, such as being on a tossing boat with no view of the horizon. Connections between regions in the brain stem and the autonomic system result in the symptoms of nausea, cold sweats, and vomiting.
The part of the brain responsible for vomiting, or emesis, is known as the area postrema. It is located next to the fourth ventricle and is not restricted by the blood–brain barrier, which allows it to respond to chemicals in the bloodstream—namely, toxins that will stimulate emesis. There are significant connections between this area, the solitary nucleus, and the dorsal motor nucleus of the vagus nerve. These autonomic system and nuclei connections are associated with the symptoms of motion sickness.
Motion sickness is the result of conflicting information from the visual and vestibular systems. If motion is perceived by the visual system without the complementary vestibular stimuli, or through vestibular stimuli without visual confirmation, the brain stimulates emesis and the associated symptoms. The area postrema, by itself, appears to be able to stimulate emesis in response to toxins in the blood, but it is also connected to the autonomic system and can trigger a similar response to motion.
Autonomic drugs are used to combat motion sickness. Though it is often described as a dangerous and deadly drug, scopolamine is used to treat motion sickness. A popular treatment for motion sickness is the transdermal scopolamine patch. Scopolamine is one of the substances derived from the Atropa genus along with atropine. At higher doses, those substances are thought to be poisonous and can lead to an extreme sympathetic syndrome. However, the transdermal patch regulates the release of the drug, and the concentration is kept very low so that the dangers are avoided. For those who are concerned about using “The Most Dangerous Drug,” as some websites will call it, antihistamines such as dimenhydrinate (Dramamine®) can be used.
 Watch this video to learn about the side effects of 3-D movies. As discussed in this video, movies that are shot in 3-D can cause motion sickness, which elicits the autonomic symptoms of nausea and sweating. The disconnection between the perceived motion on the screen and the lack of any change in equilibrium stimulates these symptoms. Why do you think sitting close to the screen or right in the middle of the theater makes motion sickness during a 3-D movie worse?
Watch this video to learn about the side effects of 3-D movies. As discussed in this video, movies that are shot in 3-D can cause motion sickness, which elicits the autonomic symptoms of nausea and sweating. The disconnection between the perceived motion on the screen and the lack of any change in equilibrium stimulates these symptoms. Why do you think sitting close to the screen or right in the middle of the theater makes motion sickness during a 3-D movie worse?
The autonomic system is affected by a number of exogenous agents, including some that are therapeutic and some that are illicit. These drugs affect the autonomic system by mimicking or interfering with the endogenous agents or their receptors. A survey of how different drugs affect autonomic function illustrates the role that the neurotransmitters and hormones play in autonomic function. Drugs can be thought of as chemical tools to effect changes in the system with some precision, based on where those drugs are effective.
Nicotine is not a drug that is used therapeutically, except for smoking cessation. When it is introduced into the body via products, it has broad effects on the autonomic system. Nicotine carries a risk for cardiovascular disease because of these broad effects. The drug stimulates both sympathetic and parasympathetic ganglia at the preganglionic fiber synapse. For most organ systems in the body, the competing input from the two postganglionic fibers will essentially cancel each other out. However, for the cardiovascular system, the results are different. Because there is essentially no parasympathetic influence on blood pressure for the entire body, the sympathetic input is increased by nicotine, causing an increase in blood pressure. Also, the influence that the autonomic system has on the heart is not the same as for other systems. Other organs have smooth muscle or glandular tissue that is activated or inhibited by the autonomic system. Cardiac muscle is intrinsically active and is modulated by the autonomic system. The contradictory signals do not just cancel each other out, they alter the regularity of the heart rate and can cause arrhythmias. Both hypertension and arrhythmias are risk factors for heart disease.
Other drugs affect one division of the autonomic system or the other. The sympathetic system is affected by drugs that mimic the actions of adrenergic molecules (norepinephrine and epinephrine) and are called sympathomimetic drugs. Drugs such as phenylephrine bind to the adrenergic receptors and stimulate target organs just as sympathetic activity would. Other drugs are sympatholytic because they block adrenergic activity and cancel the sympathetic influence on the target organ. Drugs that act on the parasympathetic system also work by either enhancing the postganglionic signal or blocking it. A muscarinic agonist (or parasympathomimetic drug) acts just like ACh released by the parasympathetic postganglionic fiber. Anticholinergic drugs block muscarinic receptors, suppressing parasympathetic interaction with the organ.
Watch this video to learn about the side effects of 3-D movies. As discussed in this video, movies that are shot in 3-D can cause motion sickness, which elicits the autonomic symptoms of nausea and sweating. The disconnection between the perceived motion on the screen and the lack of any change in equilibrium stimulates these symptoms. Why do you think sitting close to the screen or right in the middle of the theater makes motion sickness during a 3-D movie worse?
When the visual field is completely taken up by the movie, the brain is confused by the lack of vestibular stimuli to match the visual stimuli. Sitting to the side, or so that the edges of the screen can be seen, will help by providing a stable visual cue along with the magic of the cinematic experience.
A drug that affects both divisions of the autonomic system is going to bind to, or block, which type of neurotransmitter receptor?
A
A drug is called an agonist if it ________.
C
Which type of drug would be an antidote to atropine poisoning?
C
Which kind of drug would have anti-anxiety effects?
D
Which type of drug could be used to treat asthma by opening airways wider?
B
Why does smoking increase the risk of heart disease? Provide two reasons based on autonomic function.
Blood vessels, and therefore blood pressure, are primarily influenced by only the sympathetic system. There is no parasympathetic influence on blood pressure, so nicotine activation of autonomic ganglia will preferentially increase blood pressure. Also, cardiac muscle tissue is only modulated by autonomic inputs, so the conflicting information from both sympathetic and parasympathetic postganglionic fibers will cause arrhythmias. Both hypertension and arrhythmias are cardiac risk factors.
Why might topical, cosmetic application of atropine or scopolamine from the belladonna plant not cause fatal poisoning, as would occur with ingestion of the plant?
Drops of these substances into the eyes, as was once done cosmetically, blocks the muscarinic receptors in the smooth muscle of the iris. The concentration of this direct application is probably below the concentration that would cause poisoning if it got into the bloodstream. The possibility of that concentration being wrong and causing poisoning is too great, however, for atropine to be used as a cosmetic.

You can also download for free at http://cnx.org/contents/14fb4ad7-39a1-4eee-ab6e-3ef2482e3e22@11.1
Attribution: